Biology (SJCR)
Stechnolock Journal of Case Reports
Full Text
Volume 2, Issue 1
Clinical Profile, Spirometry and Respiration Related Quality of Life of Moroccan Patients with Silicosis
*Corresponding Author: Dr Senhaji L, Center of Pneumology and Silicosis, Jerada, Morocco, Tel: +212 (6) 662100560, E-mail: Dr.lamiyaesenhaji@gmail.com
doi: /sjcr.2021.2.103
Citation: Senhaji L, Karhate Andaloussi M, Germain M, Casillas JM, Ben Maamar S, et al. (2021) Clinical Profile, Spirometry and Respiration Related Quality of Life of Moroccan Patients with Silicosis. Stechnolock J Case Rep 1: 1-9
Copyright: © 2021 Senhaji L. This is an open-access article distributed under the terms of Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Silicosis is an occupational disease that is responsible for a public health problem in the city of Jerada due to persistent clandestine mining of coal mines. The aims of this study are to evaluate the impact of silicosis on the respiratory function, to assess respiration-related quality of life using the Saint George Respiratory Questionnaire (SGRQ) and to determine its influencing factors among patients with silicosis. This is a cross sectional study of 147 silicotic patients to collect socio- demographic data and to assess impairments, respiratory function (spirometry), and quality of life (SGRQ). The mean age of our patients is 64.08 years ± 6.46. Thirty-one percent had obstructive ventilatory disorder and 41.49% had a restrictive ventilatory disorder. The Hospital Anxiety and Depression Scale (HADS)revealed that 61.91% of our patients had anxiety and 83.67% had depression.TheMean SGRQ scale scores with standard deviation (sd) are as follows: Symptoms (SGS): 45.95%
± 23.66, Activity (SGA): 79.58% ± 19.8, Impacts (SGI): 68.32% ± 22.33 and Overall:68.02% ± 19.54.Our study showed the deficiencies caused by silicosis, its impact on respiratory function and the quality of life of our patients and the need to develop a respiratory rehabilitation program to improve their well-being.
Keywords: Silicosis; Rehabilitation; Quality of Life; Spirometry; Morocco
Introduction
Silicosis is a work-related disease that is widespread around the world. It is due to the inhalation of mineral dust containing silica in crystalline form. It causes chronic inflammation and progressive pulmonary fibrosis. It occurs in three forms: the most common is the chronic form, developing after more than ten years of exposure to silica dust. The accelerated form, identical to the previous one, develops after an exposure of less than 10 years [1,2]. The acute form, called silico-proteinosis, can occur after a few weeks of exposure and is associated with respiratory syndrome, fever and rapid deterioration of general health, rapidly progressing to death [3]. This disease became known on a large scale at the time of the industrial revolution with the advent of coal mining.More than three million people were exposed to silica in Europe in the 1990s but the most affected country remains China with 24,000 deaths annually in the 1990s and 600,000 cases during the same period. The annual incidence would range between 36,500 and 7,300 cases in the United States with nearly 2,700 deaths over a decade [1].
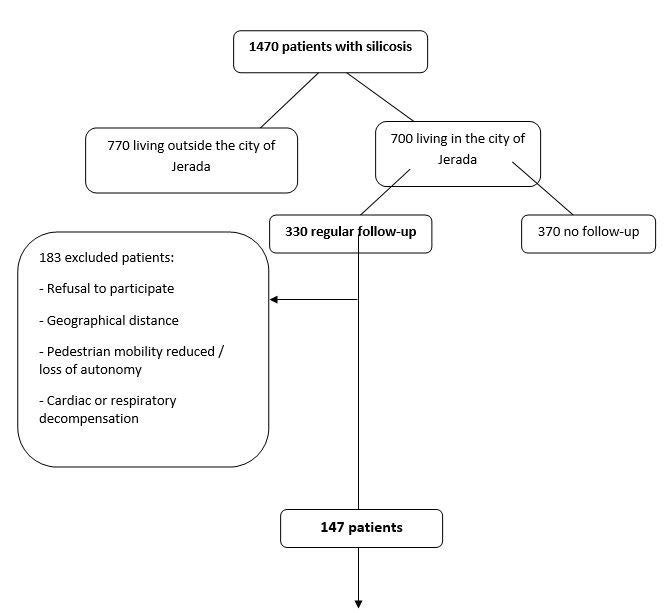
In Morocco, and precisely in the east of the country, a small town called Jerada was created in 1927 after the discovery of coal in the region. Mining activity began there in 1936 and coal from this region was considered among the best in the world. The mines closed in 1998, releasing around 9000 miners, among which 2018 were diagnosed with silicosis [4]. According to statements by the local authority, there were 1470 living persons with silicosis in 2018.Thesewere not limited to the former miners, but also included other inhabitants who resumed the coal extraction after the official closure of the mine, without appropriate protection. This clandestine mining activity practiced by the inhabitant of Jerada, is mostly motivated by poverty and the rarity of work opportunities in the city. Consequently, silicosis might remain a real public health concern and priority in the Moroccan Oriental region.
Silicosis is a chronic disease, responsible for multiple deficiencies, with respiratory, cardiovascular, muscular, psychic (anxiety, de- pression), osteo-articular (osteoporosis), nutritional and metabolic (diabetes) repercussions, leading to a significant limitation in daily living activities and a restriction of participation [5]. The aim of the current study was to evaluate the impact of silicosis on the respiratory function, to assess respiration-related quality of life and to determine its influencing factors among patients with silicosis in Morocco. To our best knowledge, this is the first Moroccan study assessing the impact of silicosis on respiratory function, and the quality of life, in order to develop a specific rehabilitation program for these patients.
Experimental section
Design and subjects
A cross-sectional design was used for this study. A survey was performed on outpatients with silicosis by face-to-face interview in the pneumology and silicosis center in Jerada between December 2017 and June 2018. Two experienced and trained investigators were employed to collect the data. The patients were informed about the nature of the study and gave their written consent to enroll. The study was approved by the ethics committee group of Sidi Mohammed Ben Abdellah University of Fez. It is important to note that all the patients in our study have a professional silicosis card and that this paper is issued to these patients by a scientific committee (pulmonologists and occupational physicians) of the city of Oujda after having analyzed a medical file encompassing clinical data, a functional respiratory exploration and a chest x-ray +/- a chest CT. The committee diagnoses silicosis and assigns a percentage of permanent partial impairment (PPI).
Out of the 330 patients diagnosed with silicosis and registered as regular patients followed up in the pneumology and silicosis center, 147 patients were finally included (Figure 1).
Measurements
Clinical characteristics related to silicosis, personal (age, sex and smoking status) and environmental factors (history of exposure to charcoal, age at first exposure, time of exposure to dust) were collected by the investigators.The permanent partial impairment index (PPI)was collected from the hospital records. PPI isa percentage expressing the importance of the after-effects which will remain per- manently and which reduce the physical capacity of a person who has suffered a work accident or an occupational disease. The Arabic
version of Hospital Anxiety and Depression Scale (HADS) [6] was used to assess the anxiety or depression. Patients with an anxiety or depression score <7 are considered asymptomatic and those with HADS score≥ 7 are noted as having anxiety and/or depression. Pulmonary function data were collected by spirometry according to the American Thoracic Society (ATS) recommendations for standardized pulmonary function report. The Modified Medical Research Council (mMRC) Dyspnea Scale used to assess dyspnea. The Moroccan version of The Saint George’s Respiratory Questionnaire (SGRQ) was used to assess respiration-related quality of life [7].
Statistical analysis
All Statistical analyses were performed using SPSS software ver. 22.0. We performed a descriptive analysis expressed in percentages and averages and a bi-varied analysis using Student’s t-test for the comparison of two means, one-way analysis of variance (ANOVA) comparing means of more than two groups, and Chi2 test to compare two percentages. P-value of 0, 05 was considered statistically significant.
Results
Basic characteristics
Table 1 presents demographics, clinical and functional characteristics as well as the Health-Related Quality of Life status of Silicotic patients. The 147 participants were all men with an average age of 64.08 ± 6.46 years [range from 46-81]. Their average time of dust exposure was 19.04 ± 7.45 years [range from 2-36]. The average duration between onset of dust exposure and early symptoms of sili- cosis was 18.07 ± 9.5 years [range from 3-42] and the average duration from onset of exposure to official disease reporting was 18.66
± 9.93 years [range from 3-45]. Forty six percent of our patients had a PPI index ≥ 70%. 46.1% of the patients were former smokers or current smokers. 39.4% had a BMI> 25 (Obesity or overweight), 6.1% were underweight. Almost 40%of our patients had co-mor- bidities such ascardiopathy (11.9%), tuberculosis (8.33%), chronic obstructive pulmonary disease (COPD) (31.97%) and chronic respiratory insufficiency (4.26%). 17.01% of our patients reported dyspnea stage 1 according to the classification of mMRC, 64.63% dyspnea stage 2, 17.01% dyspnea stage 3 and 1.35% stage 4 dyspnea. 61.91% of our patients had anxiety symptoms and 83.67% had depression symptoms.
Respiratory function
The mean forced expiratory volume in one-second (FEV1) was 2.21 ± 2.7 L (69.22 ± 27.89% of predicted) indicating moderate impairment of pulmonary function.
The mean of forced vital capacity (FVC) was 2.55±0.88L (%). 31.97% of patients had an obstructive airway disorder and 41.49% had a restrictive ventilatory disorder.
In all participants, the mean scores of symptoms, activity and impacts were 45.95±23.66, 79,58±19,8 and 68,32±22,33, respectively. The total score of the SGRQ was 68.02±19.54.
Table 2 summarizes the value of FEV 1 based on the time of silica exposure and smoking status. The average FEV1 for smokers, non- smokers and former smokers was 80.4%, 61.5% and 68.8%, respectively (p> 0.05).
Moreover, there was a statistically significant relationship between time of silicosisexposure and degree of depression: the longer the time of dust exposure, the greater the number of patients with depression (p = 0.01).
Respiration-related quality of life among patients with silicosis
Table 3 summarizes the quality of life scores of our patients, compared to their demographic and clinical data. There was no statistically significant difference in the quality of life scores based on smoking status and duration of coal exposure. In contrast, patients with a history of tuberculosis and those with COPD had a higher symptom score than those who had no tuberculosis and no history of COPD (p = 0.001 and p = 0.002 respectively). A statistically significant relationship was found between dyspnea stage, FEV1 and SRSG. Patients with anxiety symptoms had higher St George questionnaire scores compared to silicotic patients not presenting with anxiety and patients with depression had an activity score (p = 0.04) and a total score (p = 0.004) that were significantly higher than those of non-depressed patients.
The multivariate linear regression analysis on respiration- related QoL
Univariate linear regression analysis was performed with quality of life scores as reference variables. Age was associated with a high Saint George’s total score; and the onset of symptoms relative to the onset of coalexposure was related to an increased overall quality of life score. There was a correlation between PPI, FEV 1, and Saint George’s quality of life scores. Thus, the higher the PPI, the higher the Saint George questionnaire scores, was underlying a poor quality of life. In contrast, the higher the FEV1, the lower the scores reflecting a better quality of life.
Discussion
This is the first national study, conducted at the Jerada Silicosis Center to determine the clinical, functional, and health-related quality of life in silicotic patients.Our patients had a lower average age than the patients in the Chinese study of Liu et al. (73.3 years) [8] and the one of Han et al. (74.1 years) [9]. It was rather close to that of patients in the American study of Rosenman et al (69.5 years) [10] and higher than the one of the Algerian series, reporting a relatively young population (33.75 years) [11].
Only 8.3% of our patients had a history of tuberculosis, which remains a very low prevalence compared to the Chinese and Italian studies, where tuberculosis was identified in 29.3%, 67% and 22.2% of the patients respectively) [8-9, 12].46.1% of our patients were smokers or former smokers compared to 76.3% in the study of Liu et al. [8], and 50.63% in the study of Han et al. [9].In our study, the average duration of exposure to silica was 18.9 years (ranged from 2 to 36 years), while it was higher in the Chinese studies (28.6 and 27.9 years respectively) [8,9].
Inhalation of crystalline silica over prolonged periods results in impaired pulmonary function manifested by obstruction and pulmonary restriction, including a decrease in FEV 1 with a 6-minute walk test limitation [8,9,14,15]. In this study, the average FEV1 of our patients was 69.22% (ranging from 18% to 149%) indicating moderate impairment of the respiratory function. It was similar to some studies [8,10], and higher to the average FEV1 in other studies [9,10,14]. 31% of our patients had an obstructive airway disorder and 41.49% had a restrictive ventilatory disorder. In the study conducted in Iran, 4.7% of the patients had an obstructive airway disorder and 51.8% a restrictive ventilatory disorder [15]. In studies of construction workers exposed to silica, pulmonary function tends to decrease more deeply with tobacco, but when the adjustment was made for the effects of smoking, a decrease due to exposure persisted [16]. This is consistent with our findings because no significant difference was found between the FEV1 of smokers and non-smokers.
Subjective well-being and quality of life are closely related to the physical and mental state of the person [9]. The quality of life of patients with an occupational disease is considerably reduced and the level of disability cannot accurately reflect their quality of life [17]. The Saint George questionnaire showed fairly high scores which reflected a poor quality of life for our patients. This is consistent with the results of the Wang study [14] where the mean of SGT, SGS, SGA and SGI were respectively 63.8 ± 16.3; 62.3 ± 15; 62.1 ± 17.6; 66.9 ± 22.6. Other studies [13,17,18] that used other quality of life questionnaires (WHOQOL-100, SF36) showed that the quality of life of silicotic patientswas lower than control subjects.
In our study, we didn’t find a correlation between age and the total quality of life score, as well as a relationship between the onset of symptoms or the onset of exposure and the SGT contrary to other studies [17,18]. Also, our data did not show a link between the duration of exposure and the quality of life of our patients unlike the results of Liu’s study [9].
Conclusion
Our study has shown that the clinical and functional status of patients with silicosis is deleterious and that they have a poor quality of life. Hence, it is highly recommended that these patients be included in a respiratory rehabilitation program as soon as possible in order to help them prolong their survival and improve their quality of life.
Acknowledgements
We would particularly like to thank the 147 patients who so generously gave up their time totake part in this study
- Leung CC, Sun Yu IT, Chen W (2008) Silicosis. Lancet 379: 2008-18.
- Cullinan P, Reld P (2013) Pneumoconiosis. Prim Care Respir J 22: 249-52.
- Racil H, Ben Salema N, Chaoucha N, Ismail O, CheikhRouhoua S, et al. (2012) Silicoproteinosis: a radioclinical entity apart [La silicoprotéinose : une entité radioclinique à part]. Rev Mal Respir 29: 1132-6.
- Jerada (2019) Wikipédia (https://fr.wikipedia.org/wiki/Jerada, consulté en février 2019), France.
- Brichet A, Tillie-Leblond I, Wallaert B, Tonnel AB (2016) Silicosis and pneumoconiosis of the coal miner. Medico-surgical ency- clopedia 6-039-T-60 [Silicose et pneumoconiose du mineur de charbon. Encyclopédie médico-chirurgicale 6-039-T-60].
- El Rhazi K, Nejjari C, Serhier Z, Tachfouti N, Berraho M, et al. (2009) Difficulties of transcultural adaptation of health measure- ment scales in southern countries: example of the validation of the St-George Respiratory Questionnaire in Morocco [Difficultés de l’adaptation transculturelle des échelles de mesureen sante´ dans les pays du sud : exemple de la validationdu St-George Respiratory Questionnaire au Maroc]. Rev Epidémio et Santé Publique 57: 179-89.
- Bendahhou K, Serhir Z , Ibrahim Khalil A, Radallah D , Amegrissi S, et al .(2014) Validation of the Moroccan dialect version of the scale [Validation de la version dialectale Marocaine de l’échelle] « HADS ». Rev Epidémioet Santé Publique 65:S53.
- Liu H, Yan B, Han B, Sun J, Yang Y, et al. (2011) Assessment of respiration-related quality of life of Chinese patients with silicosis and its influencing factors using the St. George’s Respiratory Questionnaire (SGRQ). Journal of Clinical Nursing.Blackwell Publish- ing Ltd, USA.
- Han B, Yan B, Zhao N, Zhang J, Sun J, et al. (2013) The influence of the functional capacity on subjective well-being and quality of life of patients with silicosis. Aging and Mental Health.
- Rosenman KD, Reilly MJ, Gardiner J (2010) Results of spirometry among individuals in a silicosis registry. JOEM 52: 12.
- Aberkane S (2017) Perceived health related quality of life outcomes with silicosis patients. Iran J Public Health 46: 1299-300.
- Galietti F, Giorgis GE, Oliaro A, Ardizzi A, Miravalle C, et al. (1989) Lung diseases associated with silicosis: Study of 618 cases. Minerva Med 80: 987-90.
- Yildiz T, Eşsizoğlu A, Önal S, Ateş G, Akyildiz L, et al. (2011) Quality of life, depression and anxiety in young male patients with silicosis due to denim sandblasting. TüberkülozveToraksDergisi 59: 120-5.
- Cheng W, Lin-Sheng Y, Xiao-He S, Yu-Fu Y, Kui L, et al. (2008) Depressive symptoms in aged Chinese patients with silicosis. Aging and Mental Health 12: 343-8.
- Rushton L (2007) Chronic obstructive pulmonary disease and occupational exposure to silica. Reviews on Environmental Health 22.
- Tavako E, Azari M, Zendehdel R, Salehpour S, Khodakrim S, et al. (2017) Risk evaluation of construction workers’ exposure to silica dust and the possible lung function impairments. Tanaffos 16: 295-303.
- Li H, Lin M, Zhang W, Li J, Zou J (2015) Relation entre qualité de vie et niveau d’incapacité chez les patients atteints de maladie professionnelle. Zhonghua Lao Dong Wei Sheng Zhi et Bing ZaZhi 33: 735-8.
- Cheng W (2015) Quality of life and influencing factors for patients with silicosis: an analysis of 220 cases.. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing ZaZhi 33: 116-8.