Biology (SJCR)
Stechnolock Journal of Case Reports
Full Text
Volume 2, Issue 1
Irreductible Giant Inguinoscrotal Hernia with Bowel Contents Assimilated to a Sliding Hernia: a Case Report
*Corresponding Author: Ndambwe Moussio VAS, Surgery and specialities department, Faculty of Medical and biomedical sciences, Yaounde I University, Yaounde I Teaching Hospital, Cameroon, Tel: +237 697 87 44 83, E-mail: vickyaudrey47@yahoo.fr
doi: /sjcr.2021.2.101
Citation: Ndambwe Moussio VAS, Guifo ML, Ngoundjou A, Ekanga T, Kamla Igor, et al. (2021) Irreductible Giant Inguinoscrotal Hernia with Bowel Contents Assimilated to a Sliding Hernia: a Case Report. Stechnolock J Case Rep 2: 1-8
Copyright: © 2021 Ndambwe Moussio VAS. This is an open-access article distributed under the terms of Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
In Africa, frequently, inguino-scrotal hernias are found amongst the most common surgical pathologies. The management of giant hernia is difficult because of many factors: the reduction can lead to abdominal compartment syndrome (called loss of domain), mesh repair is almost necessarily required and the aesthetic challenge related to the residual scrotal volume. We report on a 60-year-old patient with a recurrent giant left-sided inguinoscrotal hernia. A Lichtenstein mesh repair associated with a scrotal skin reduction was done. We found the entire omentum, small and large bowel in the hernia sac. The patient presented an abdominal compartment syndrome encompassing a sub-intestinal obstruction, jaundice and infection of the surgical site as post-operative complications. We will discuss the value of prior abdominal preparation in our context and bowel or omental resection during the repair.
Keywords: Giant Hernia; Sliding Hernia; Abdominal Compartment Syndrome
Introduction
An inguinoscrotal hernia is a very common surgical pathology. An inguinoscrotal hernia is defined as a giant one, if the neck is greater than 10 cm and/or when the hernia extends beyond the midpoint of the inner thigh in an upright position [1,2]. Anand et al. classified it into 3 types [2]: Type I, at the midpoint of the thigh; type II, between mid-thigh and the supra-patellar line; and type III beyond the patella. Sliding hernias are rare with 2 - 5% incidence. A sliding hernia is a protrusion through an abdominal wall opening, in a retroperitoneal organ, with or without its mesentery, with or without an adjacent peritoneal sac [3,4]. According to Bendavid, there are three types of sliding hernias, it is probably simplest to call them types I, II, and III in descending order of frequency [5]: Type I: is the type of hernia in which part of the peritoneal sac is made up by the wall of a viscera (95% of sliding hernias). It's sac contains sigmoid, caecum and appendix mostly and rarely ileum or the annex in the girl and uterus; Type II: any hernia containing a retroperitoneal viscera and its mesentery, in which the mesentery forms part of the wall of the peritoneal sac (5% of sliding hernias), mostly, it sac contains sigmoid colon and rarely caecum, appendix or schedule; Type III: a protrusion of the viscera itself; the peritoneal sac may be very small or even absent (is the rarest type and is found in only one of 10,000 herniae). This type of hernia is the most treacherous type and the opening of the sac is exposed to the lesion of the viscera. It has been described as an extraperitoneal, sacless and extrasaccular sliding hernia.
Giant hernias are said to have a different physiological impact. We progressively observe the reduction of intra-abdominal pressure which leads to venous stasis in splanchnic and inferior vena cava circulation, intestinal dilatation with associated hypo-motility. These hernias also cause a modification of the respiratory mechanics by the loss of function of the abdominal accessory respiratory muscles [6].
The technical difficulties in repairing inguinoscrotal hernias are related to the restoration of anatomical structures, function and aesthetics of the groin region. Perioperative complications are caused by comorbidities often present and by physiological changes due to loss of the domain of abdominal viscera [7]. The significant increase in intra-abdominal pressure secondary to viscera reintegration may be the cause of abdominal compartment syndrome requiring a particular preoperative pneumoperitoneum [6], or resection of digestive structures present in the hernia sac [7].
We had a report on a 60-year-old patient with a recurrent giant left-sided inguinoscrotal hernia. A Lichtenstein mesh repair associated with a scrotal skin reduction has been done and we found the entire omentum, small and large bowel in the hernia sac. We will discuss the value of abdominal preparation in our context and the prior bowel or omental resection during the repair.
Case report
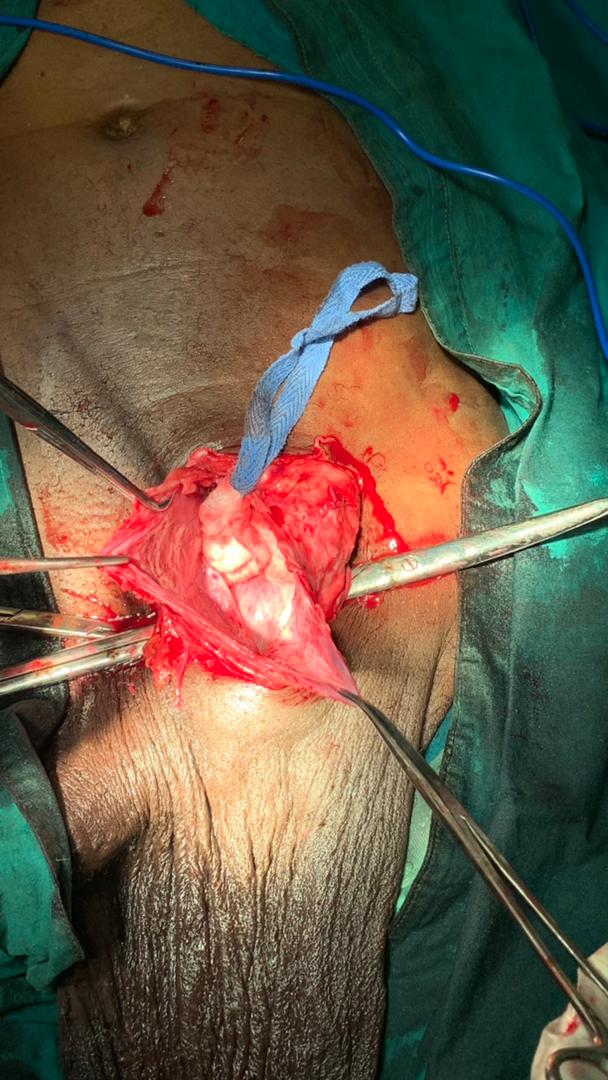
A 60 years – old patient, an industrial worker, with a history of industrial smoke inhalation for about 30 years ago with sequel fibrosis of the lower lobe of the right lung; who have presented a huge recurrent left-sided inguinoscrotal hernia for 14 years. A herniorraphy was done in a rural health centre and the recurrence occurs 3 months later. On a physical examination (Figure 1), there was a large left inguinoscrotal hernia descending to the knee, not painful, not impulsive, but irreducible with a neck measuring approximately 10 cm, the right testis was palpable but the left was difficult; auscultation of the inguinal tumefaction reveals bowel sounds. Biological pre-operative work-up was normal. A pulmonary chest X-ray showed right base atelectasis, but the patient did not have any respiratory symptoms like cough, wheeze or breathlessness. Electrocardiogram (ECG) was normal. Due to financial constraints, the abdominal, Computerized Tomography (CT) scan was not done, so as to specify the anatomy of the abdominal wall, as well as the hernia contents in order to carry out the volumetric measurements of the sac. Also, no preoperative preparation had been made to reduce the risk of abdominal compartment syndrome. However, the patient was admitted and a manoeuver to manually reduce the hernia content was done to promote the rehabilitation of the patient to the abdominal position of viscera; but the reduction was often incomplete. The patient was booked for surgery. The anaesthetic team preferred spinal anaesthesia over general anaesthesia because of the presence of atelectasis in the preoperative period. A transverse incision on the inferior abdominal line parallel to Langer's line was done. There was dehiscence of the external oblique aponeurosis. The cord was then separated from the sac and dissection was kept close to the spermatic cord. The adherences of the sac with the deep inguinal ring were dissected. There was attempt to reduce the hernia sac content that wasn’t successful, hence, the sac was opened carefully at its thinnest point and it was found to contain the whole colon and whole of ileum with its mesentery as its content also. Posteriorly, to our surprise, the caecum, appendix and ascending colon were found to be part of the sac (Sliding hernia type I) (Figure 2). The contents within the sac were reduced. Only part of the sac, which was thin, was removed, leaving the posterior part formed by the caecum, appendix and ascending colon. No digestive structures were resected (Figure 3). A polypropylene prosthesis measuring 15cm x 15cm was placed using the Lichtenstein technique and resection of the excess scrotal skin was made at the same operating time associated with scrotal drainage by a lamella drain. The patient was observed for 24 hours in the Intensive Care Unit (ICU).
The operative aftermath was marked by:
- On the local level: Superficial discharge of the inguinal operative site was managed on daily basis by dressing with the removal of 2 stitches and deep infection of the scrotal site 7 days after the operation which leads to the removal of all the stitches and drain with daily surgical debridement and dressing. Forty (40) days after the operation, a secondary suture was made on the scrotum (Figures 4,5 and 6).
- On loco-regional and general level: 3 days after the operation, the patient developed signs of abdominal compartment syndrome encompassing: sub intestinal occlusion (diffuse abdominal pain, abdominal meteorism, no gas, and no stool), respiratory distress and jaundice. Liver check-ups and measurement of intra-abdominal pressure has not been done because of the lack of finances, but medical management was done which includes a nasogastric tube, prokinetics to promote intestinal emptying, hyperhydration and electrolyte balance and oxygen therapy. The amelioration of the clinical state occurred progressively with a normal intestinal transit 14 days after the operation.
The patient was discharged 31 days after the operation.
Discussion
Giant groin hernias are common in Africa [8]. Where populations, especially rural populations let hernia evolve several years before seeking for medical attention; this can be due to poor access to basic health care or due negligent attitude and fear of surgical procedure in our settings. Our patient waited 14 years before consulting because of the functional burdens of the hernia which has critically reduced his daily activities. Giant hernia results in the weakening of the posterior wall of the inguinal canal, giving way to a gaping deep inguinal ring with significant visceroptosis [8]. The chronic nature of the disease poses a challenge to the patient after the intervention; because the reduction of hernia contents in the abdominal cavity can lead to a sharp increase in Intra-Abdominal Pressure (IAP), a reduction of venous return and a decrease in diaphragm motility responsible for respiratory distress. Tidal volume reduction, post-operative ileus, and abdominal compartment syndrome are potential immediate post-operative complications. There are many strategies to increase abdominal compliance before the reintegration of hernia contents; among them, we have the pre-operative progressive pneumoperitoneum, the use of “Expander” and more recently, the application of botulin toxin [6]. During the intervention, viscera resection (colon, ileum, kidney, omentum…) can be done to assure the reduction of hernia contents without tension in the abdominal cavity [7]. Another therapeutic alternative after the intervention is to keep the patient under mechanical ventilation for about 10 days after the hernia content is replaced in the abdominal cavity [9].
In our case, no pre-operative abdominal preparation has been made in order to prevent abdominal compartment syndrome; and no viscera resection was done during the intervention; this can explain why in the immediate post-operative period, our patient presented signs of abdominal compartment syndrome which was managed medically. Indeed, before surgical decompression (which remains the only defined management for abdominal compartment syndrome) is considered, a less invasive optional medical treatment can be envisaged. It is based on five different mechanisms: the improvement of abdominal compliance, the evacuation of intraluminal content, the evacuation of abdominal fluid collections, the correction of capillary leaks and a positive water balance and, finally, specific treatments [10].
The frequency of sliding hernias increases with patient age. It is almost nil before the age of 30 and increases to 20% after the age of 70 [11]. Our patient was 60 years old, which is within the favourable age group. The diagnostic of sliding hernia is done intraoperative.
Studies have reported the use of the Bassini technique to repair giant inguinoscrotal hernias [12], or the prosthetic cure as Lichtenstein technique [13]; but these studies do not report short term recurrences. Because of the enlargement of the deep inguinal ring and the defect of the musculoaponeurotic structures found in giant inguinoscrotal hernias, it seems appropriate to use a prosthetic cure for the wall reinforcement. The omentectomy involved in a smaller increase in intra-abdominal pressure reduction is preferred to intestinal resection as it helps to prevent post-operative complications. The left intra-scrotal position of the caecum and ascending colon raises the question of the non-fixation of the later in the form of a common mesentery as the congenital mechanism, and if not congenital, it deserves to be elucidated from a physiopathological point of view. This situation could explain post-operative occlusive syndrome seen in our case and this leads to the discussion of the benefit of hemicolectomy as prevention of abdominal compartment syndrome and post-operative transit disorders.
The scrotal surplus is a real aesthetic problem and the attitude to adopt is not uniform. We had opted for a resection of this surplus, which can explain the cascade of local infection after surgery. Many studies proposed a reductive scrotal plastic surgery to reduce the risk of local complications and aesthetic problems [14]. In a study done by Diop et al. in Senegal, they choose a conservation of scrotal skin and testicle in their patients and observed a spectacular retraction of the scrotum in short term [8]; such as Mehendal et al. who recommend conservation of the scrotal surplus which can serve as an “anatomical silo” to receive the abdominal content in case of early recurrence or severe respiratory problems [7].
Conclusion
The treatment of giant inguinal hernias constitutes a challenge for the surgeon, especially in a precarious environment. Abdominal hyper pressure which follows the reduction of hernia content is one of the main problems to be faced. Every patient with such a hernia should be systematically prepared before the intervention and the surgeon should be ready for viscera sacrifice. Anticipation and prevention of mechanical difficulties do not guarantee a non-eventful follow-up and calls for collaboration and a multidisciplinary approach.
Conflict of Interest Statement: None declared
Authors Contributions
➢ NDAMBWE MOUSSIO V.: Conceptualization, methodology
➢ NGOUNDJOU Amanda: Data curation, writing original draft preparation
➢ GUIFO Marc Leroy / NDAMBWE / NGOUNDJOU / EKANGA: Supervision, writing-reviewing and editing
➢ Guy-Aristide BANG / SAVOM Patrick / Biwole Daniel / KAMLA Igor / Arthur ESSOMBA: Validation
- Trivedi D, Trompetas V, Karavias D (2021) Giant sliding inguinoscrotal hernia causing megaureter and large bowel obstruction. J Gastrointest Surg (2021).
- Anand M, Hajong R, Naku N, Hajong D, Singh K (2017) Giant inguinal herniae managed by primary repair: a case series. J Clin Diagn Res 11: PR01-2.
- Sahoo M, Kumar T (2013) Sliding hernia with appendix, cecum, ascending colon forming sliding component and transverse colon and greater omentum forming contents of the sac: A case report. Int J Case Report Images 4: 123–6.
- Medico-surgical encyclopedia; surgical treatment digestive system; surgical treatment of inguinal hernias via the inguinal route [Encyclopédie médico-chirurgicale ; traitement chirurgical appareil digestif ; traitement chirurgical des hernies inguinales par voie inguinale ; 2017].
- Bendavid R (2002) Sliding hernias, article in Hernia October 6: 137-40.
- Balaphas A, Morel P, Breguet R (2016) Giant hernias with loss of citizenship: how to best prepare patients? [Hernies géantes avec perte de droit de cité : comment préparer au mieux les patients ?] Rev Med Suisse 12: 1170-3.
- Mehendal F, Taams K, Kingsnorth A (2000) Repair of a giant inguinoscrotal hernia. Br J Plast Surg 53: 525-9.
- Sall DBI (2011) Management of giant inguinal hernias: about five observations [Prise en charge des hernies inguinales géantes : à propos de cinq observations]. Médecine et Santé Tropicales 23: 30-4.
- Ouazzani A (2009) A large inguinoscrotal hernia [une volumineuse hernie inguinoscrotale]. Rev Med Brux 30: 189-91.
- Manu L, Malbrain G (2011) Abdominal compartment syndrome [le syndrome du compartiment abdominal], MAPAR.
- Sourav S (2016) A Case Report of Sliding Inguinal Hernia Containing Ascending Colon, Caecum and Whole of Ileum with its Mesentery as its Content. Hellenic Journal of Surgery 88: 433-5.
- Savoie P, Abdalla S, Bordes J (2014) Surgical repair of giant inguinoscrotal hernias in an austere environment: leaving the distal sac limits early complications. Hernia 18: 113-8.
- Tarchouli M, Ratbi M, Bouzroud M (2015) Giant inguinoscrotal hernia containing intestinal segments and urinary bladder successfully repaired by simple hernioplasty technique: a case report. J Med Case Rep 9: 276.
- Merrett N, Waterworth M, Green M (1999) Repair of giant inguinoscrotal inguinal hernia using marlex mesh and scrotal skin flaps. Aust N Z J Surg 64: 380-3.